We offer a comprehensive line of vascular access products that help to ensure you have the right vascular access device for each and every patient. These products are available in a variety of sizes and design configurations.
> To jump to a specific product webpage quickly, use the buttons below.

View each product’s Instructions for Use, specifications, components, and other resources by clicking the links below.

Infections hurt your patients, your HAC score, your bottom line, and much more. Help is here with Cook Spectrum technology.
 The right combination
The right combination
Cook Spectrum catheters are impregnated with a combination of the antibiotics minocycline and rifampin in order to help patients by providing proven protection against catheter-related bloodstream infections (CRBSIs).¹
 Unmatched evidence
Unmatched evidence
The efficacy of Cook Spectrum is supported by more than 30 sources published over the past two decades, including peer-reviewed studies and meta-analyses.
 No evidence of increased resistance
No evidence of increased resistance
More than 10 years of clinical use and a 7-year study of more than 500,000 Cook Spectrum catheter days have shown no evidence of increased antibiotic resistance.²
 Worth switching
Worth switching
Switching from unimpregnated catheters to Cook Spectrum catheters helps provide quality patient care by decreasing the risk for CRBSIs and the costs associated with treating them.1,3
View a comprehensive list of Cook Medical products that have Cook Spectrum technology.


〉Available with or without Cook Spectrum technology
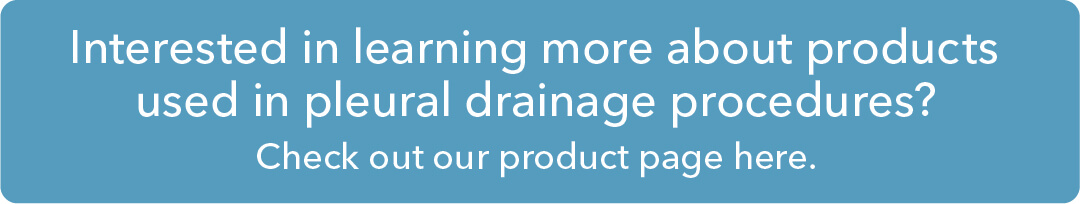
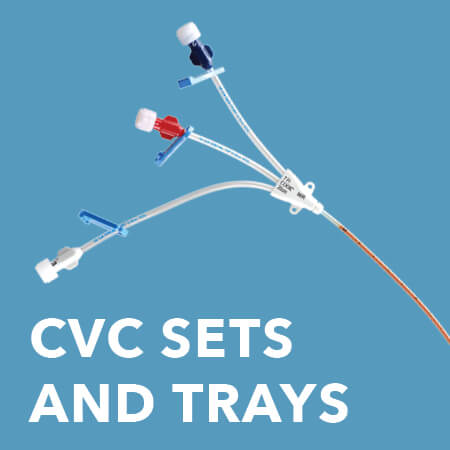
Used for treatment of critically ill patients and suggested for continuous or intermittent drug infusions; central venous blood pressure monitoring (CVP); acute hyperalimentation; blood sampling; delivery of whole blood or blood products; and simultaneous, separate infusion of drugs.
Features and benefits
• Cook Spectrum central venous catheters (CVCs) provide patients with proven protection against CRBSIs.1
• Power-injectable (CT) options are available; “CT” is printed on the distal lumen.
• Depth markings every 1 cm help you insert the acute CVC accurately.
• Maximum flow rates are printed on the lumen clamps.
• The polyurethane material is designed for pushability and high flow rates.
• A wide variety of sizes maximizes your procedural options.
View more details about CVC sets and trays and Cook Spectrum CVCs.

Used as an alternative to intravenous access during pediatric emergencies, permitting the infusion of drugs and fluids.
Features and benefits
• Two laterally opposed sideports positioned near the needle cannula’s distal tip ensure proper flow if the needle tip is obstructed by posterior bone cortex.
• The positioning mark that is 1 cm proximal to the needle cannula’s distal tip provides a visual reference point for depth determination.
View more details about the Dieckmann Intraosseous Infusion Needle.

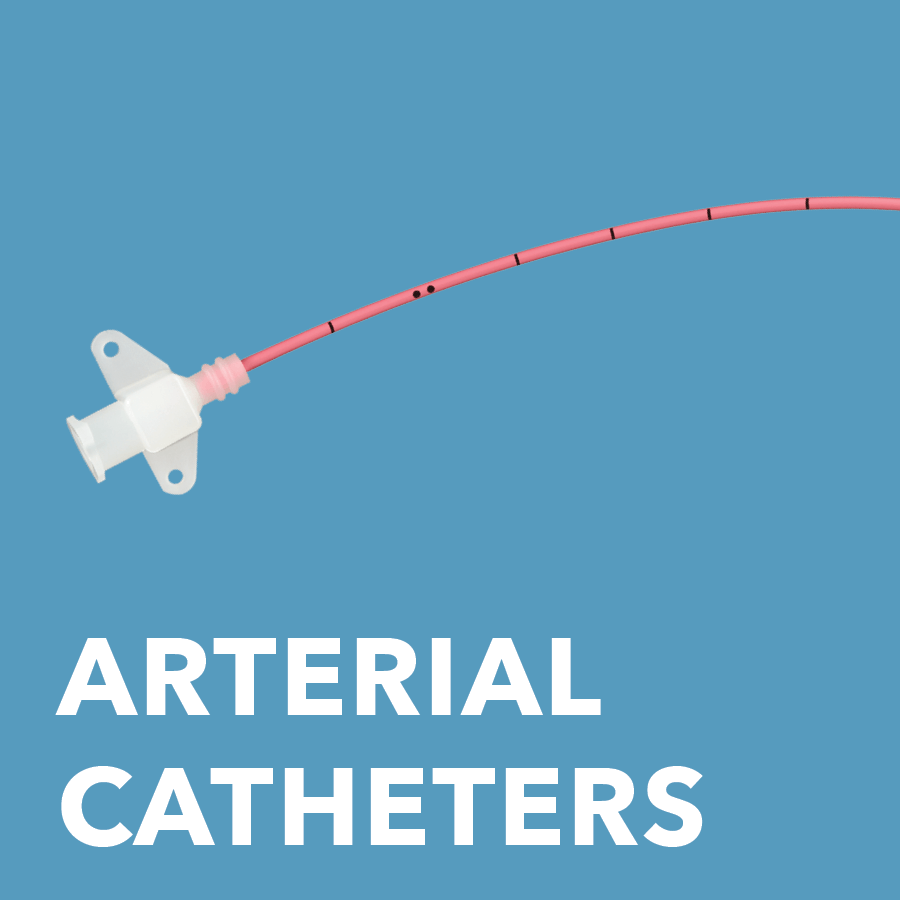
Used for arterial pressure monitoring and blood sampling.
View more details about Arterial Pressure Monitoring Sets and Trays.

Used for the retrieval of venous air emboli.
Features and benefits
• Seldinger placement facilitates controlled, minimally invasive catheter introduction.
• The entire catheter is radiopaque in order to maximize visibility during placement under an x-ray.
View more details about the Bunegin-Albin Air Aspiration Set.
1. Raad I, Darouiche R, Dupuis J, et al. Central venous catheters coated with minocycline and rifampin for the prevention of catheter-related colonization and bloodstream infections: a randomized, double-blind trial. Ann Intern Med. 1997;127(4):267-274.
2. Ramos ER, Reitzel R, Jiang Y, et al. Clinical effectiveness and risk of emerging resistance associated with prolonged use of antibiotic-impregnated catheters: more than 0.5 million catheter days and 7 years of clinical experience. Crit Care Med. 2011;39(2):245-251.
3. Zimlichman E, Henderson D, Tamir O, et al. Health care-associated infections: a meta-analysis of costs and financial impact on the US health care system. JAMA Intern Med. 2013;173(22):2039-2046.
Contact A Representative
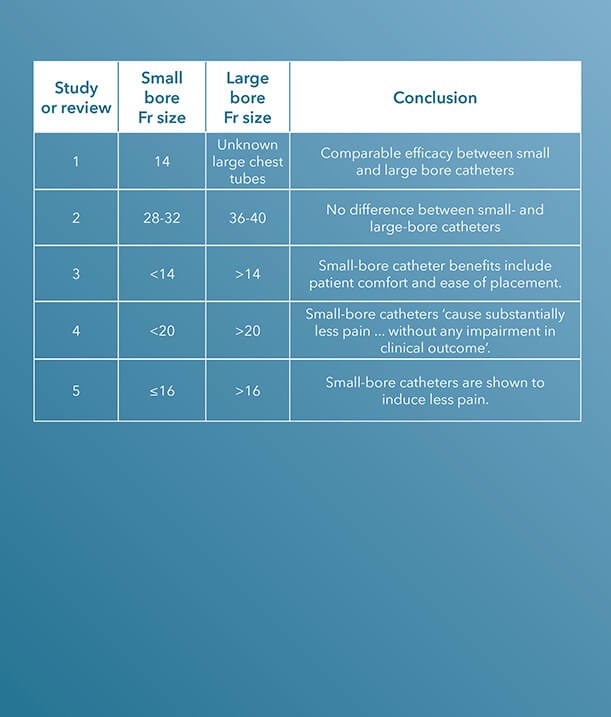
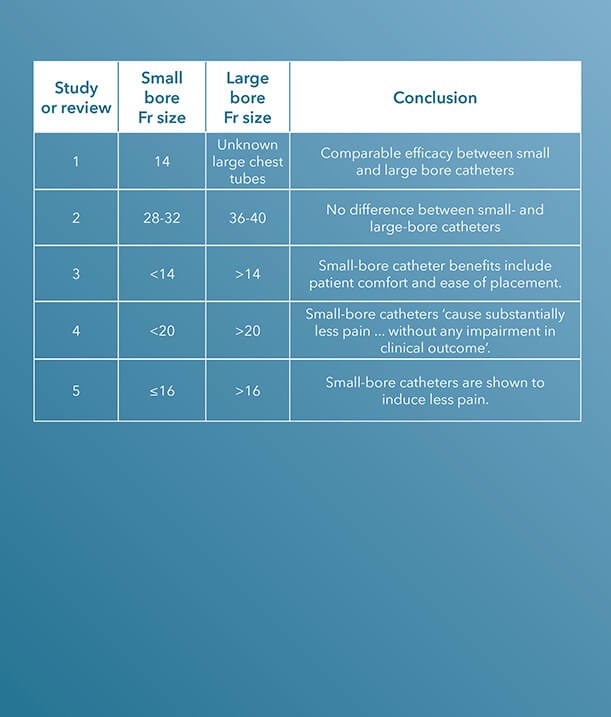
Since 1963, Cook Medical has been a champion of minimally invasive treatment options for patients. In the case of the centesis and drainage procedural areas, the healthcare industry discussion has largely centered around the efficacy of large-bore versus small-bore catheters.
Within the last decade, there have been several clinical studies and review articles published in peer-reviewed journals stating the increased efficacy and improvement of small-bore catheters versus large-bore catheters for pleural and pericardial drainage procedures.
To see Critical Care’s entire product portfolio of small-bore chest tubes for pleural and pericardial drainage, click here.
ARTICLE 1 (STUDY)
“Two-year experience of using pigtail catheters to treat traumatic pneumothorax: a changing trend,” published in The Journal of Trauma in 2011, is a study comparing small-bore, 14 Fr pigtail catheters to chest tubes in patients with nontraumatic pneumothoraces.
A chest tube, “because of its large caliber and significant trauma during an insertion, can cause pain, prevent full lung expansion, and worsen pulmonary outcome. Pigtail catheters (PC)… are smaller and less invasive,” the introduction to the study states.¹
The charts of 9,624 trauma patients over a two-year period at a Level I trauma center were evaluated. The study concludes that the “demographics, tube days, need for mechanical ventilation, and insertion-related complications were similar,” using these characteristics to determine that pigtail catheters have a comparable efficacy to chest tubes.1
ARTICLE 2 (STUDY)
36 to 40 Fr chest tubes were also compared to small-bore pigtail catheters in a similar study also published in The Journal of Trauma and Acute Care Surgery, titled “Does size matter? A prospective analysis of 28-32 versus 36-40 French chest tube size in trauma.”
There was no difference in the efficacy of drainage [or] rate of complications.2
In this study, the authors claim that “the optimal chest tube size for the drainage of traumatic hemothoraces and pneumothoraces is unknown.”2 This study was designed to compare the efficacy of small-bore versus large-bore drainage catheters in patients with thoracic trauma.
Data were gathered on 293 patients who required open chest tube drainage within 12 hours of admission to a Level I trauma center.
“Clinical demographic data and outcomes including efficacy of drainage, complications, retained hemothoraces, residual pneumothoraces, need for additional tube insertion, video-assisted thoracoscopy, and thoracotomy were collected and analyzed by tube size,” the authors indicate.2 Small-bore catheters, ranging from 28 to 32 Fr, were compared with large chest tubes, ranging from 36 to 40 Fr; a total of 353 catheters, 186 small and 167 large, were placed during the study.
The authors determined that “the need for tube reinsertion, image-guided drainage, video-assisted thoracoscopy, and thoracotomy” are the same when comparing small-bore to large-bore catheters.2
“For injured patients with chest trauma, chest tube size did not impact the clinically relevant outcomes tested. There was no difference in the efficacy of drainage, rate of complications including retained hemothorax, need for additional tube drainage, or invasive procedures,” the study concludes.2
ARTICLE 3 (REVIEW)
In 2013, a paper published in Clinics in Chest Medicine aimed to generalize the use of small-bore catheters for drainage procedures, including in pleural infection.
In “Straightening out chest tubes: what size, what type, and when,” the authors state that “small-bore tubes (<14 Fr) are effective for most pleural processes. Various types of pneumothorax and malignant and infected complicated pleural effusions have been successfully managed with small-bore chest tubes.”3
Abundant literature supports a paradigm shift towards the more routine use of small-bore chest tubes for managing pleural disease.3
The authors also state that the benefits of using small-bore drainage catheters include patient comfort and ease of catheter placement.3
The study concludes that “abundant literature supports a paradigm shift towards the more routine use of small-bore chest tubes for managing pleural disease.”3
ARTICLE 4
A study published in CHEST, titled “The relationship between chest tube size and clinical outcome in pleural infection,” aimed to determine the optimal choice of drainage catheter sizes for pleural infection.
This multicenter study enrolled 405 patients and evaluated “the combined frequency of death and surgery, and secondary outcomes,” specifically “hospital stay, change in chest radiograph, and lung function at 3 months,” in patients who received a variety of sizes of chest tubes. In 128 of the 405 patients, a pain scale was also included.4
“There was no significant difference in the frequency with which patients either died or required thoracic surgery in patients receiving chest tubes of varying sizes,” the study notes; however, “pain scores were substantially higher in patients receiving (mainly blunt dissection inserted) larger tubes.”4
The study concludes that “smaller, guide-wire-inserted chest tubes cause substantially less pain than blunt-dissection-inserted larger tubes, without any impairment in clinical outcome in the treatment of pleural infection.”4
ARTICLE 5 (REVIEW)
Although the precise optimal chest drain size remains unknown, a review article titled “Optimal chest drain size: the rise of the small-bore pleural catheter,” published in Seminars in Respiratory and Critical Care Medicine, asserts that “objective data supporting the use of large-bore [chest] tubes is scarce.”5
The onus now is on those who favor large tubes to produce clinical data to justify the more invasive approach.5
In support of the efficacy of small-bore drains, the article states, “Increasing evidence shows that small-bore catheters induce less pain and are of comparable efficacy to large-bore tubes, including in the management of pleural infection, malignant effusion, and pneumothoraces. The onus now is on those who favor large tubes to produce clinical data to justify the more invasive approach.”5
Interested in chatting with a Cook Medical representative?
Please submit the required information to connect with your local Cook representative. This form is intended for US-based physicians only. Please see our Privacy Statement for data protection notices relating to our collection and use of your data.
1. Kulvatunyou N, Vijayasekaran A, Hansen A, et al. Two-year experience of using pigtail catheters to treat traumatic pneumothorax: a changing trend.
J Trauma. 2011;71(5):1104-1107.
2. Inaba K, Lustenberger T, Recinos G, et al. Does size matter? A prospective analysis of 28-32 versus 36-40 French chest tube size in trauma. J Trauma Acute Care Surg. 2012;72(2):422-427.
3. Mahmood K, Wahidi MM. Straightening out chest tubes: what size, what type, and when. Clin Chest Med. 2013;34(1):63-71.
4. Rahman NM, Maskell NA, Davies CW, et al. The relationship between chest tube size and clinical outcome in pleural infection. Chest. 2010;137(3):536-543.
5. Fysh ET, Smith NA, Lee YC. Optimal chest drain size: the rise of small-bore pleural catheter. Semin Respir Crit Care Med. 2010;31(6):760-768.
Contact A Representative
We offer an extensive line of chest tubes for removing both air and fluid from the pleural and pericardial spaces. These products are available in a variety of designs and sizes, including several small-bore configurations, Seldinger and trocar options, and sets and trays to meet specific procedural preferences. View each product’s indications for use, specifications, components, and other resources by clicking the links below.
Pneumothorax catheters
 Used for the relief of simple, spontaneous, iatrogenic, and tension pneumothorax.
Used for the relief of simple, spontaneous, iatrogenic, and tension pneumothorax.
Features and benefits
• Seldinger placement facilitates controlled, minimally invasive catheter introduction.
• The set comes with the Cook Chest Drain Valve, which is designed to help remove air from the pleural cavity.
• The enlarged sideports are designed to facilitate the drainage of air.
• The radiopaque catheter material enhances x-ray visualization.
• Pigtail catheters have a comparable efficacy to chest tubes in patients with pneumothorax.*
*Kulvatunyou N, Vijayasekaran A, Hansen A, et al. Two-year experience of using pigtail catheters to treat traumatic pneumothorax: a changing trend. J Trauma. 2011;71(5):1104–1107.
View more details about the Wayne Pneumothorax Catheter Set and Tray – Seldinger.
 Used for the relief of simple, spontaneous, iatrogenic, and tension pneumothorax.
Used for the relief of simple, spontaneous, iatrogenic, and tension pneumothorax.
Features and benefits
• The needle obturator comes pre-assembled within the Wayne Pneumothorax Catheter to allow for direct-stick insertion.
• The set comes with the Cook Chest Drain Valve, which is designed to help remove air from the pleural cavity.
• The enlarged sideports are designed to facilitate the drainage of air.
• The radiopaque catheter material enhances x-ray visualization.
• Pigtail catheters have a comparable efficacy to chest tubes in patients with pneumothorax.*
*Kulvatunyou N, Vijayasekaran A, Hansen A, et al. Two-year experience of using pigtail catheters to treat traumatic pneumothorax: a changing trend. J Trauma. 2011;71(5):1104–1107.
View more details about the Wayne Pneumothorax Catheter Set – Trocar.
 Used for emergency relief and temporary management of suspected tension pneumothorax.
Used for emergency relief and temporary management of suspected tension pneumothorax.
Features and benefits
• The set comes with the Cook Chest Drain Valve, which is designed to help remove air from the pleural cavity.
View more details about the Cook Emergency Pneumothorax Set.
 Used for the relief of simple, spontaneous, or iatrogenic pneumothorax and tension pneumothorax.
Used for the relief of simple, spontaneous, or iatrogenic pneumothorax and tension pneumothorax.
Features and benefits
• The straight catheter is used for trocar placement.
• The radiopaque catheter material enhances x-ray visualization.
• The set and tray come with a vinyl connecting tube and a three-way stopcock.
• The set comes with the Cook Chest Drain Valve, which is designed to help remove air from the pleural cavity.
View more details about the Pneumothorax Set and Tray.
 Used for the relief of simple, spontaneous, or iatrogenic pneumothorax and tension pneumothorax.
Used for the relief of simple, spontaneous, or iatrogenic pneumothorax and tension pneumothorax.
Features and benefits
• Seldinger placement facilitates controlled, minimally invasive catheter introduction.
• The 8.5 Fr catheter is designed for smaller patient anatomies.
• Sideports are positioned within the catheter pigtail and are designed to aid in drainage.
• The set comes with the Cook Chest Drain Valve, which is designed to help remove air from the pleural cavity.
View more details about the Richli Pneumothorax Catheter Set.
 Used for the relief of simple, spontaneous, or iatrogenic pneumothorax and tension pneumothorax.
Used for the relief of simple, spontaneous, or iatrogenic pneumothorax and tension pneumothorax.
Features and benefits
• Seldinger placement facilitates controlled, minimally invasive catheter introduction.
• The radiopaque catheter material enhances x-ray visualization.
View more details about the Catheter Aspiration Set for Simple Pneumothorax.
Multipurpose catheters
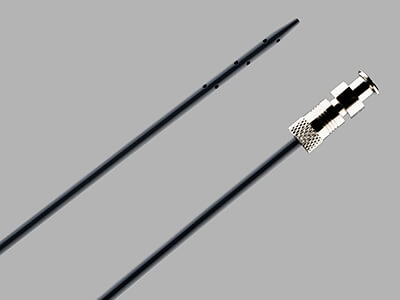
 Used for the percutaneous introduction of a chest tube for pleural fluid drainage.
Used for the percutaneous introduction of a chest tube for pleural fluid drainage.
Features and benefits
• Seldinger placement facilitates controlled, minimally invasive catheter introduction.
• The centimeter-marked dilators allow for additional control over the insertion of a chest tube into the pleural space.
• The sideports are positioned at the distal end of the chest tube.
• The clear polyvinylchloride catheter with a radiopaque stripe allows fluid to be seen during the drainage procedure.
• The most proximal side hole is positioned on the radiopaque stripe to aid in confirming catheter positioning via x-ray.
• The double lumen set has an additional lumen available for aspiration or infusion.
• The Thal-Quick Chest Tube Adapter is sold separately.
View more details about the Thal-Quick Chest Tube Set and Tray.

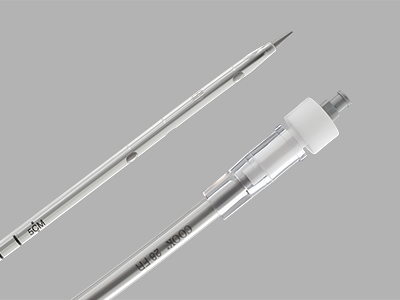
After percutaneous insertion via the Seldinger technique, the pigtail catheter of the Fuhrman Pleural Drainage Set serves as a conduit to drain air or fluid from the pleural space to outside the body.
Features and benefits
• Seldinger placement facilitates controlled, minimally invasive catheter introduction.
• The catheter is available in a variety of sizes, ranging from 5 to 12 Fr, to cater to different patient anatomies.
• Sideports are positioned within the catheter pigtail and are designed to aid in drainage.
• Centimeter markings on the pigtail catheter guide insertion.
• The catheter material has radiopaque properties.
• Pigtail catheters have been shown to have a comparable efficacy to chest tubes in patients with pneumothorax.*
*Kulvatunyou N, Vijayasekaran A, Hansen A, et al. Two-year experience of using pigtail catheters to treat traumatic pneumothorax: a changing trend. J Trauma. 2011;71(5):1104–1107.
View more details about the Fuhrman Pleural/Pneumopericardial Drainage Set and Tray.
Pericardiocentesis catheters
 Used to remove fluid from the pericardial sac.
Used to remove fluid from the pericardial sac.
Features and benefits
• Seldinger placement facilitates controlled, minimally invasive catheter introduction.
• The 40 cm long catheter is designed to cater to larger patient anatomies.
• The radiopaque catheter material enhances x-ray visualization.
View more details about the Lock Pericardiocentesis Set and Tray.

Used to infuse or withdraw rinsing solutions in the peritoneal cavity.
Features and benefits
• Seldinger placement facilitates controlled, minimally invasive catheter introduction.
• The catheter is equipped with 90 sideports.
• The radiopaque catheter material enhances x-ray visualization.
View more details about the Peritoneal Lavage Set and Tray.
Accessories
 Used in conjunction with a pneumothorax aspiration catheter if incomplete expansion of the lung persists after mechanical aspiration of air.
Used in conjunction with a pneumothorax aspiration catheter if incomplete expansion of the lung persists after mechanical aspiration of air.
Features and benefits
• The set comes with the Cook Chest Drain Valve, which is designed to help remove air from the pleural cavity.
View more details about the Simple Pneumothorax Aspiration Accessory Set.
 Used for connection to other medical devices such as catheters.
Used for connection to other medical devices such as catheters.
Features and benefits
• The adapter is male Luer lock to a universal taper.
View more details about the Multipurpose Plastic Tubing Adapter.
 Used for the connection of an external drainage catheter to a drainage pouch.
Used for the connection of an external drainage catheter to a drainage pouch.
View more details about the Vinyl Connecting Tube.
 Used to provide separate sampling or an infusion port within Thal-Quick chest tubes.
Used to provide separate sampling or an infusion port within Thal-Quick chest tubes.
Features and benefits
• This accessory is compatible with the Thal-Quick Chest Tube Set and Tray.
View more details about the Thal-Quick Chest Tube Adapter.
Interested in chatting with a Cook Medical representative?
Please submit the required information to connect with your local Cook representative. This form is intended for US-based physicians only. Please see our Privacy Statement for data protection notices relating to our collection and use of your data.
Lung ultrasound is a necessary, key component in both pulmonary and critical care settings due to its high diagnostic accuracy and physicians’ ability to perform it at the bedside. In cases of pleural disease, lung ultrasound could be an essential component of care, from the initial diagnosis through clinical management and treatment.
Last year, Cook Medical had two physicians with expertise in the use of thoracic ultrasound for pleural disease share recent advances of this technique at two major industry conferences: the European Respiratory Society (ERS) International Congress and the CHEST Annual Meeting.

ERS International Congress
Luigi Vetrugno, MD, is a Professor of Anaesthesia and Intensive Care at the University Hospital of Udine in Udine, Italy. In his presentation, Thoracic ultrasound for pleural effusion, he discussed several studies he has published in recent years about the important role ultrasound plays in diagnosing and treating pleural effusion.
“Ultrasound plays a significant role in the education of physicians,” Dr. Vetrugno said. “They will need to be trained to view this technology as an extension of their senses, just as many generations have viewed the stethoscope in a similar way.”
In one study co-authored by Dr. Vetrugno and published in Critical Care Medicine, thoracic ultrasound is said to not only help physicians visualize pleural effusion, but also to help them distinguish between the different types that can be present.1
Additionally, “TUS [thoracic ultrasound] is essential during thoracentesis and chest tube drainage as it increases safety and decreases life-threatening complications. It is crucial not only during needle or tube drainage insertion, but also to monitor the volume of the drained PLEFF [pleural effusion].”1
An observational study co-authored by Dr. Vetrugno assessed “the prevalence of complications related to ultrasound-guided percutaneous small-bore pleural drain insertion.”2
He stated that “small-bore pleural drainage device insertion has become a first-line therapy for the treatment of pleural effusions.” In this study, ultrasound was used to assess the safety and complication rates in patients with pleural effusions. The study’s authors found ultrasound-guided placement to be a “safe procedure,” however, in the future, estimating the amount of pleural effusion by ultrasound will be necessary to standardize the procedure. The authors also concluded that for resident physicians “training and proficiency assessment should be formalized.”2
An additional article by Dr. Vetrugno in favor of ultrasound guidance can be found in Critical Ultrasound Journal, Respiratory and Pulmonary Medicine, and Annals of Intensive Care.
 He has also submitted letters to the editor regarding the importance of patient position during ultrasound procedures.
He has also submitted letters to the editor regarding the importance of patient position during ultrasound procedures.
In one letter, Dr. Vetrugno advised for the patient to remain in supine position with a mild torso elevation of 15 degrees, not a semi-recumbent position with the torso at 40-45 degrees as previous authors stated.3 “This means that as fluid follow the law of gravity, an overestimation of the maximal distance between partial and visceral pleura could be obtained,” he said. This theory “overestimates in tall males with large thoracic circumference small effusions under 200 mL and in large ones above 1000 mL.”3
According to Dr. Vetrugno, this equation allows for a high mean prediction error, however, it is recognized that “an urgent standardization of the method to assess PLEFF [pleural effusion fluid] with lung ultrasound is needed to reach a definite conclusion.”3
In another letter to the editor, Dr. Vetrugno echoed his concerns that larger and more standardized clinical studies should be performed before a definite conclusion is reached.4
CHEST Annual Meeting
Seth Koenig, MD, FCCP, is the Director of Education and Professor of Medicine in the Division of Pulmonary Medicine at Montefiore Medical Center in New York City, New York. In his presentation, Ultrasonography for the diagnosis and management of pleural disease, he presented about the extensive benefits of using ultrasound, most notably regarding patient safety.
Dr. Koenig started his presentation with an important question, “How do we maximize the things we can do for our patients safely without using another service? And how does ultrasound help?”
To this question, the majority of the physician audience said that they routinely use ultrasound for general purposes, however, Dr. Koenig urged them to consider ultrasound for pleural effusions. “For me, I use ultrasound to do everything,” he said.
 Dr. Koenig explained that the use of ultrasound prevents a concept commonly known as “clinical and time dissociation.”
Dr. Koenig explained that the use of ultrasound prevents a concept commonly known as “clinical and time dissociation.”
“When you ask for another service, you invoke the ancient art of clinical and time dissociation,” he said. “For example, if you ask for a CAT scan, you will most likely have to involve a surgeon, an infectious disease doctor, and a pulmonologist. This can be confusing for the patient. Someone else reads the exam, you get the results of that exam, but they’re not intimately involved in the patient. This takes time for the exams to come in, plus, you have to move the patient. Is this what you do, or should we figure out a better way?”
Ultrasound, according to Dr. Koenig, not only provides added clarity in terms of a diagnostic approach, but it may also reduce the number of specialists involved in the diagnostic process.
“Every single patient that we see from the pulmonary and from critical care departments gets an ultrasound,” he said.
Additional advantages of ultrasound, according to Dr. Koenig, include:
- Short learning curve
- Portable; the patient does not need to be transferred
- Decrease the need for chest x-rays
- Vessels are visible; helps to avoid post-procedural bleed
- Can reduce likelihood of a visceral laceration, vascular injury, or pneumothorax
- Ability to monitor and record complications
Dr. Koenig also said that using ultrasound alleviates the need to precisely place a chest tube in the “triangle of safety,” a small, preferred site of insertion as determined by the British Thoracic Society.5
“The triangle isn’t a problem anymore,” he said. “As long you have a nice space, you can stick the needle wherever is convenient for you and the patient because you can see everything. As long as you know where you are and your wire guide is well placed, it doesn’t matter what you insert after. The point is, if you can see it, you can do something about it.”
Dr. Koenig ended his lecture by emphasizing the most important reason physicians should consider the use of ultrasound for pleural diseases: the patients.
“We have to think about our patients before we do things,” he said. “In 2019, I believe patients see too many doctors. They get a doctor for this, they get a doctor for that, what happens is, patients get really confused, and so if you can decrease the number of people and the number of procedures that a person has, they thank you for it, believe it or not. In conclusion, ultrasound is good for the patient, but it’s also good for you. Ultrasound helps with diagnostic and therapeutic planning. It helps to diagnose complications. It’s helpful to follow the progress of a pleural effusion, and it’s obviously extremely good for documenting post-procedure pneumothoraces.”
Dr. Vetrugno is not a paid consultant of Cook Medical.
Dr. Koenig is a paid consultant of Cook Medical.
1. Brogi E, Gargani L, Bignami E, et al. Thoracic ultrasound for pleural effusion in the intensive care unit: a narrative review from diagnosis to treatment. Crit Care. 2017;21:325.
2. Vetrugno L, Guadagnin GM, Barbariol F, et al. Assessment of pleural effusion and small pleural drain insertion by resident doctors in an intensive care unit: an observational study. Clin Med Insights Circ Respir Pulm Med. 2019;13: 1179548419871527.
3. Vetrugno L, Bove T. Lung ultrasound estimation of pleural effusion fluid and the importance of patient position. Ann Intensive Care. 2018;8:125.
4. Vetrugno L, Brogi E, Barbariol F. “A message in the bottle.” Anesthesiology. 2018;128(3):677.
5. Griffiths JR, Roberts N. Do junior doctors know where to insert chest drains safetly? Postgrad Med J. 2005;81:456-458.
 The right combination
The right combination Unmatched evidence
Unmatched evidence No evidence of increased resistance
No evidence of increased resistance Worth switching
Worth switching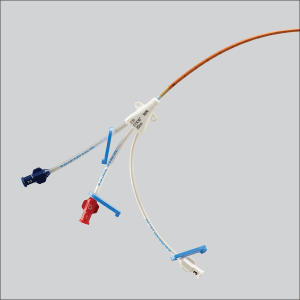 CVC sets and trays
CVC sets and trays Dieckmann Intraosseous Infusion Needle
Dieckmann Intraosseous Infusion Needle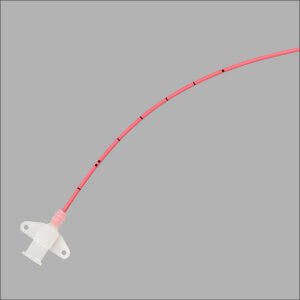 Arterial Pressure Monitoring Sets and Trays
Arterial Pressure Monitoring Sets and Trays Bunegin-Albin Air Aspiration Set
Bunegin-Albin Air Aspiration Set






 Used for the relief of simple, spontaneous, iatrogenic, and tension pneumothorax.
Used for the relief of simple, spontaneous, iatrogenic, and tension pneumothorax. Used for the relief of simple, spontaneous, iatrogenic, and tension pneumothorax.
Used for the relief of simple, spontaneous, iatrogenic, and tension pneumothorax. Used for emergency relief and temporary management of suspected tension pneumothorax.
Used for emergency relief and temporary management of suspected tension pneumothorax. Used for the relief of simple, spontaneous, or iatrogenic pneumothorax and tension pneumothorax.
Used for the relief of simple, spontaneous, or iatrogenic pneumothorax and tension pneumothorax. Used for the relief of simple, spontaneous, or iatrogenic pneumothorax and tension pneumothorax.
Used for the relief of simple, spontaneous, or iatrogenic pneumothorax and tension pneumothorax. Used for the relief of simple, spontaneous, or iatrogenic pneumothorax and tension pneumothorax.
Used for the relief of simple, spontaneous, or iatrogenic pneumothorax and tension pneumothorax. Used for the percutaneous introduction of a chest tube for pleural fluid drainage.
Used for the percutaneous introduction of a chest tube for pleural fluid drainage.
 Used to remove fluid from the pericardial sac.
Used to remove fluid from the pericardial sac.
 Used in conjunction with a pneumothorax aspiration catheter if incomplete expansion of the lung persists after mechanical aspiration of air.
Used in conjunction with a pneumothorax aspiration catheter if incomplete expansion of the lung persists after mechanical aspiration of air. Used for connection to other medical devices such as catheters.
Used for connection to other medical devices such as catheters. Used for the connection of an external drainage catheter to a drainage pouch.
Used for the connection of an external drainage catheter to a drainage pouch. Used to provide separate sampling or an infusion port within Thal-Quick chest tubes.
Used to provide separate sampling or an infusion port within Thal-Quick chest tubes.
 He has also submitted letters to the editor regarding the importance of patient position during ultrasound procedures.
He has also submitted letters to the editor regarding the importance of patient position during ultrasound procedures. Dr. Koenig explained that the use of ultrasound prevents a concept commonly known as “clinical and time dissociation.”
Dr. Koenig explained that the use of ultrasound prevents a concept commonly known as “clinical and time dissociation.”