A 73-year-old patient was referred to us with a “painless” obstructive jaundice and pruritus secondary to a solid lesion of the pancreas. The patient was admitted to our unit with MRI and CT-scan imaging of a solid lesion of the head of the pancreas with signs of vascular involvement of mesenteric vessels and bile duct obstruction and no certain metastasis. The patient’s underlying diseases were diabetes and hypertension. A blood test showed: AST 168 U/L, ALT 79 U/L, γ-GT 1066 U/L, ALP 650 U/L, total Bilirubin 21.52 mg/dL, and dir. Bil. 14.54 mg/dL.
Under deep sedation with propofol, the patient underwent ERCP that failed for a tight stricture of the second part of the duodenum. During the procedure we decided to place a duodenal 6 cm Evolution stent (Cook Medical EVO-22-27-6-D) after a measurement of the length of stenosis with the guide catheter (Cook Medical SIS-10). The deployment of the Evolution stent under fluoroscopy was comfortable as usual.
After two days an ERCP was technically unsuccessful as the papilla was inaccessible despite probing within the duodenal stent. Thus, EUS-guided puncture was performed transgastrically into the left intrahepatic ducts. A linear array echoendoscope was placed near the gastric lesser curve allowing visualization of a dilated left hepatic duct.
To continue reading this article, download the PDF here.
Dr. Francesco Di Matteo was not a paid consultant of Cook Medical at the time of this publication.
 800.457.4500
800.457.4500
Sign Up. Get Email about News, Products, and Events from Cook Medical.

 Indication for procedure
Indication for procedure
The laparoscopic resection of colorectal carcinomas is, more and more, replacing open surgery. This minimally invasive method shows equal oncological results with less perioperative pain, a better cosmetic result, and a shortened period of recovery. A contraindication for the laparoscopic procedure is an ileum with dilated intestinal loops, because of an increased risk for perforation. Here, a preoperative stenting with colorectal metal stents offers the opportunity to relieve the ileus and to perform a minimally invasive resection later.
About the author and facility
For the past 17 years, Dr. Michael Hünerbein has performed all current endoscopic examinations and interventions, including gastroscopy, colonoscopy, and ERCP. The Helios-Hospital Berlin has longstanding experience in stenting, including colorectal stents. The hospital is certified as a reference center for surgical endoscopy by the German Society of Surgery.
Device and accessories
A standard colonoscope and a fluoroscope are used in this procedure. For the x-ray image, a water-soluble contrast is used. The stenosis is probed using a guide wire with a hydrophilic tip. Over the wire guide, an uncovered Evolution Colonic Controlled-Release Stent (available in lengths of 6, 8, or 10 cm) is pushed through the stenosis. The distal end of the stent is deployed and the positioning rectified, as the situation requires. When positioned correctly, the stent can be fully deployed.
To continue reading this article, download the PDF here.
Refer to the Evolution® Colonic Controlled-Release Stent – Uncovered product page for the complete Instructions for Use.
Dr. Michael Hünerbein was not a paid consultant of Cook Medical at the time of this publication.
 800.457.4500
800.457.4500
Sign Up. Get Email about News, Products, and Events from Cook Medical.

Globally, colorectal cancer (CRC), also known as colon cancer, is the fourth most common cause of cancer-related death. But the fact is, CRC is one of the most preventable cancers. Either people aren’t being informed, or they’re not taking the time to get screened by scheduling a colonoscopy. It’s estimated that 23 million adults (1 in 3 adults between the ages of 50 and 75) don’t have a colonoscopy as recommended. If screened in time, CRC can be treated before it’s too late. We can start by spreading the word about CRC and the importance of a colonoscopy.
 What is colorectal cancer (CRC)?
What is colorectal cancer (CRC)?
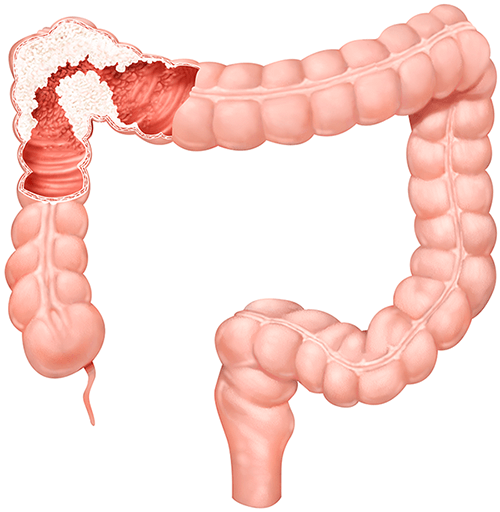
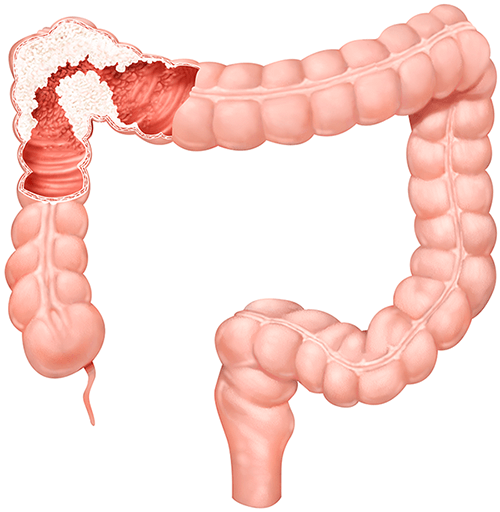
CRC is a form of cancer that develops in the colon or the rectum. It is caused by a non-cancerous adenoma or polyp growing on the inner lining of the large intestine. Over the course of many years, a non-cancerous polyp may eventually develop into cancer. However, it should be noted that not all polyps will develop into cancer.
Key statistics about CRC
- It is the second most common cancer diagnosed in women.
- It is the third most common cancer diagnosed in men.
- It accounts for almost 900,000 deaths annually.
Causes and risks
Although anyone can develop CRC, those with a family history of it have a greater risk of developing CRC in their lifetime. Lifestyle factors such as diet, weight, and exercise can also contribute to an individual’s risk of developing this type of cancer. Making healthy lifestyle choices can greatly reduce the chance of developing CRC.
Symptoms
- A change in bowel habits, including diarrhea, constipation, or narrowing of the stool, that lasts more than a few days
- Rectal bleeding with bright red blood
- Bloody stool
- Cramping or abdominal pain
- Weakness and fatigue
- Unintended weight loss
If experiencing these symptoms, contact a healthcare professional.
Colorectal cancer is preventable, treatable, and beatable.
In addition to ulcers, tumors, and areas of inflammation, a colonoscopy can also identify pre-cancerous polyps. The average colonoscopy only takes about 30 minutes and only needs to be performed every 10 years. A colonoscopy is a simple screening. And it just may be the first step to beating this cancer once and for all.
—
References:
 The COVID-19 pandemic has dramatically impacted the volume and treatment options for physicians around the world. As a result, many healthcare facilities received recommendations to suspend elective medical procedures, which has made a dramatic impact on services like preventive cancer screenings.1 In the United States alone, an analysis of electronic health record data from 39 health systems estimated that colorectal cancer (CRC) screening volumes decreased by 86% compared to screening volumes before the onset of the pandemic.2 While screening rates continue to rise, they have not yet returned to historic levels.3
The COVID-19 pandemic has dramatically impacted the volume and treatment options for physicians around the world. As a result, many healthcare facilities received recommendations to suspend elective medical procedures, which has made a dramatic impact on services like preventive cancer screenings.1 In the United States alone, an analysis of electronic health record data from 39 health systems estimated that colorectal cancer (CRC) screening volumes decreased by 86% compared to screening volumes before the onset of the pandemic.2 While screening rates continue to rise, they have not yet returned to historic levels.3
The American Society for Gastrointestinal Endoscopy (ASGE) understands the value of colonoscopies and the role they play in the treatment of colorectal cancer. We’re proud to support their initiative to provide medical professionals and patients with resources to learn more about the importance of early screening for colorectal cancer, different screening methods, and other pertinent facts.

Sources
- Gupta S, Lieberman D. Screening and surveillance colonoscopy and COVID-19: avoiding more casualties. Gastroenterology Web site. https://www.gastrojournal.org/article/S0016-5085(20)34932-5/fulltext. Published July 16, 2020. Accessed March 3, 2021.
- Delayed cancer screenings. Epic Health Research Network Web site. https://ehrn.org/articles/delays-in-preventive-cancer-screenings-during-covid-19-pandemic. Published May 4, 2020. Accessed March 3, 2021.
- Delayed cancer screenings—a second look. Epic Health Research Network Web site. https://ehrn.org/articles/delayed-cancer-screenings-a-second-look/. Published July 17, 2020. Accessed March 3, 2021.

 800.457.4500
800.457.4500
 Indication for procedure
Indication for procedure
 What is colorectal cancer (CRC)?
What is colorectal cancer (CRC)?