The COVID-19 pandemic has changed the way physicians are thinking about patient care, forcing them to adapt to new technologies and protocols. It has also given physicians the opportunity to think about the future of medicine, including what it may look like after COVID-19. Through this blog series, we’re interviewing physicians to share their first-hand experiences on how they’re adapting their practices during the COVID-19 pandemic, as well as their thoughts on the future of patient care.
 For this post we interviewed Dr. Brandon Isaacson, to get his perspective on patient care and what the protocols for otologic procedures have looked like during the COVID-19 pandemic. Dr. Isaacson is a professor in the Department of Otolaryngology—Head and Neck Surgery at UT Southwestern Medical Center and serves as co-director of UT Southwestern’s Comprehensive Skull Base Program. Below are some highlights of the interview.
For this post we interviewed Dr. Brandon Isaacson, to get his perspective on patient care and what the protocols for otologic procedures have looked like during the COVID-19 pandemic. Dr. Isaacson is a professor in the Department of Otolaryngology—Head and Neck Surgery at UT Southwestern Medical Center and serves as co-director of UT Southwestern’s Comprehensive Skull Base Program. Below are some highlights of the interview.
Cook: What impact has COVID-19 had on otologic procedures?
Dr. Isaacson: Initially, when the pandemic started in March 2020, all elective surgical procedures were placed on hold. Our facility resumed otologic surgical procedures in May 2020, testing all patients for COVID prior to surgery. N95 masks and appropriate PPE were provided for all staff in the operating room regardless of a negative preoperative COVID test. Surgical volumes were progressively increased from May through June until we were back at pre-pandemic levels, using the same preoperative COVID testing protocols and PPE requirements.
Appropriate PPE was worn in the clinic for all aerosol-generating procedures, but pre-procedure COVID testing was not performed. At present, we are still performing otologic procedures using the same testing and PPE protocols that were initiated at the beginning of the pandemic.
How are you currently prioritizing cases?
We have been at full OR capacity since early this year. We did have a brief slowdown at Children’s and the county hospital during the January COVID surge.
How have otologic procedures changed due to COVID-19 in your specific practice?
Clinic in-person visits are back to pre-pandemic levels. We have increased our use of telemedicine, which was significant at the beginning of the pandemic. At the beginning of the pandemic, I was seeing approximately 20 patients per week via telemedicine, which is now down to 4 to 6 telemedicine visits per week.
How are physical examinations being performed, if at all?
We have been performing relevant physical exams since we reinitiated in-person clinic visits in May 2020.
Is the room setup any different?
Vigorous sterilization procedures are performed in each exam room after each visit. If an aerosol-generating procedure (AGP) is performed, the room is closed afterwards.
How have you implemented PPE into your practice?
We have all been wearing face masks and using hand washing, gloves, and eye protection for each in-person encounter.
How are you screening patients for COVID-19?
Each outpatient is screened with a temperature check and a COVID-19 symptoms inventory at check-in.
The COVID-19 pandemic, which resulted in the postponement of elective procedures and has led to new COVID testing protocols and PPE requirements, has also caused otolaryngologists to take a closer look at their procedures in an effort to reduce exposure risks. Ayache et al. recently discussed the benefits of a minimally invasive endoscopic approach as an alternative to mastoidectomy and highlighted the benefits of transcanal endoscopic ear surgery (TEES) as a means to treat many otologic conditions, avoiding the risks associated with aerosol-generating procedures.1
If a virus like SARS-CoV-2 is present during a mastoidectomy, the viral particles may aerosolize and present an increased risk of transmission to the OR staff.1 Rather than making an incision behind the ear and drilling through bone to access the ear canal, TEES utilizes a rigid endoscope through the ear canal to access the middle ear, thus minimizing the risk of exposure.
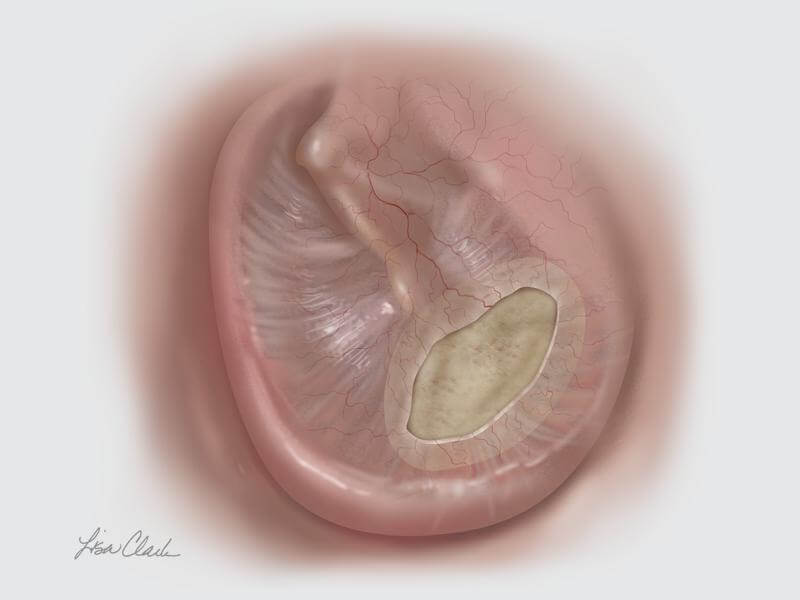 When faced with a tympanic membrane perforation, TEES can be used in conjunction with the Biodesign® Otologic Repair Graft to avoid the need for an external incision. The Biodesign Otologic Repair Graft is an off-the-shelf alternative to autologous tissue and, when paired with the endoscope, allows for a minimally invasive approach to tympanic membrane repair.
When faced with a tympanic membrane perforation, TEES can be used in conjunction with the Biodesign® Otologic Repair Graft to avoid the need for an external incision. The Biodesign Otologic Repair Graft is an off-the-shelf alternative to autologous tissue and, when paired with the endoscope, allows for a minimally invasive approach to tympanic membrane repair.
- Ayache S, Kutz W, Isaacson B, et al. COVID‑19 and ear endoscopy in otologic practices. Eur Arch Otorhinolaryngol. 2021;278(6):2133-2135.
