Five key components to providing comprehensive care for patients with aortic dissections.
BY SUKGU HAN, MD, MS, AND FERNANDO FLEISCHMAN, MD
Aortic dissections make up a significant portion of aortic emergencies that can be rapidly fatal. Time-dependent mortality and morbidity associated with aortic dissections highlight the importance of prompt, accurate evaluation and treatment for successful patient outcomes. Recent advances in endovascular technology have enabled a wide array of less invasive therapeutic options for aortic dissections. These rapidly evolving endovascular options may result in further expansion of indications for intervention. Recent approval of the Zenith Dissection System (Cook Medical) is an example of pathology-specific devices with a potential to significantly impact the natural history of aortic dissections. Consequently, optimal care of patients with aortic dissections requires multidisciplinary expertise in both open and endovascular repairs at centers with established resources and infrastructure to offer rapid treatment.1-3
To improve care for these patients, dedicated aortic centers have begun to emerge. The ability to offer complex open ascending and arch reconstructions for type A aortic dissections, as well as expertise in endovascular therapy in arch, descending, and thoracoabdominal aortic segments for type B aortic dissections, is essential for such centers to be truly comprehensive. At most centers, this skill set resides across cardiac and vascular surgery specialties. Furthermore, synergistic partnership of cardiac and vascular surgeons who are dedicated to aortic pathologies is only the first element of forming a successful aortic center. There are five additional key components that we have found to be helpful in building a true cross-disciplinary aortic program at the Keck Medical Center. They include (1) development of dedicated aortic expertise, (2) establishment of a dedicated “aortic hotline” and rapid transport system, (3) raising regional awareness through outreach efforts, (4) development of multidisciplinary aortic case conferences, and (5) development of a multidisciplinary follow-up clinic and surveillance program. In addition to describing these five components, we aim to share our experience in overcoming common roadblocks to a successful, truly collaborative partnership.
1. DEVELOPMENT OF DEDICATED AORTIC EXPERTISE
Implementing a “Shared Concentrated Experience” Model
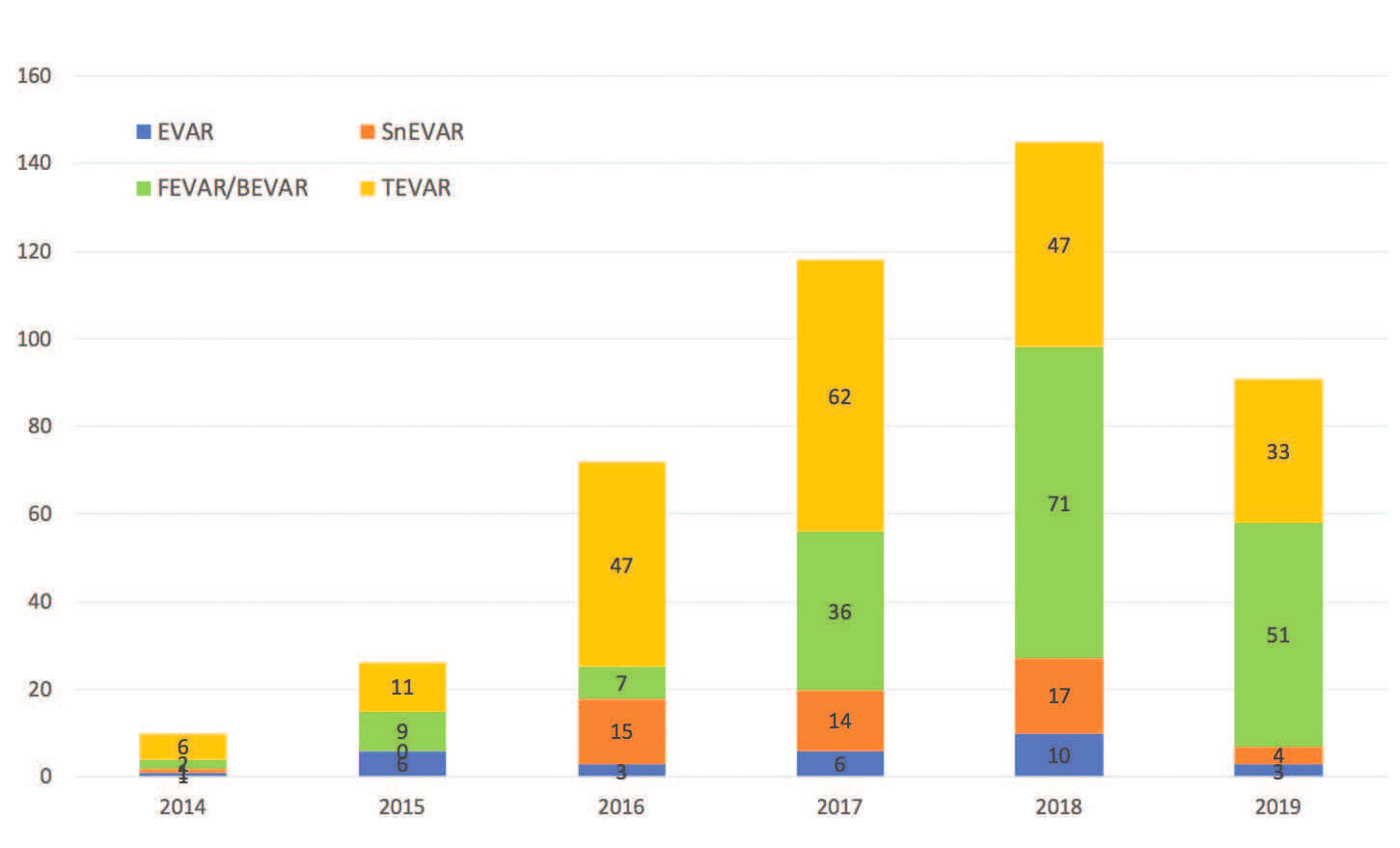
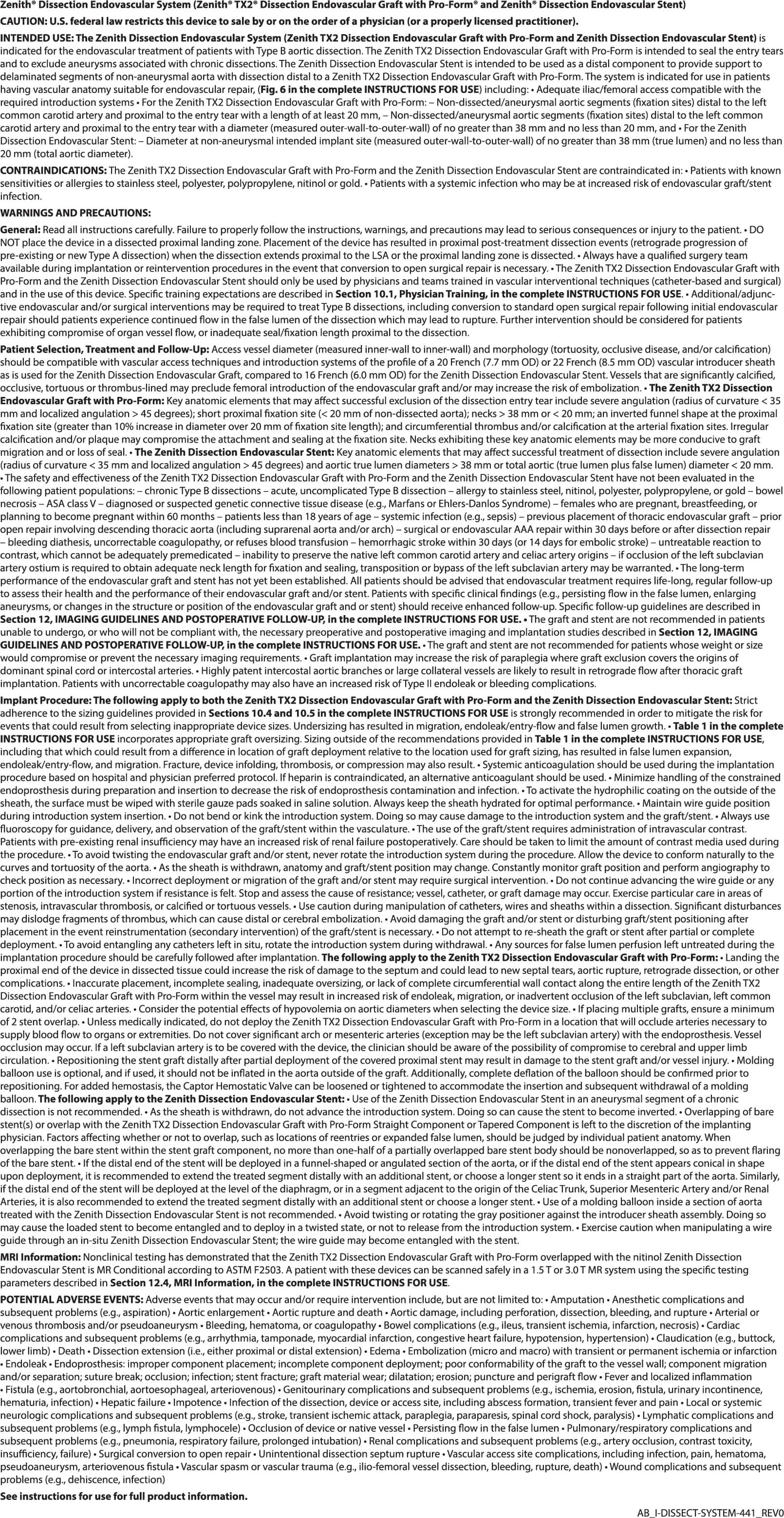
Figure 1. Growth in endovascular aortic experience in a single dedicated complex endovascular aortic surgeon by year, achieved through a shared concentrated experience model (year 2019 includes 6-month period). BEVAR, branched endovascular aneurysm repair*; FEVAR, fenestrated endovascular aneurysm repair; SnEVAR, snorkel endovascular aneurysm repair.
* These treatment options may not be available in all regions.
Overcoming the learning curve to reach expertise in both complex open and endovascular aortic repairs (EVARs) takes time and experience. When our aortic center was starting in 2012, we were performing simple thoracic endovascular aortic repairs (TEVARs), limited hybrid arch reconstructions, and infrarenal EVARs. Particularly, endovascular branch incorporations were seldom performed. Recognizing the need to rapidly develop expertise in these areas, the vascular surgery division assigned a single surgeon with a strong focus in complex endovascular aortic procedures to be the dedicated specialist. All partners within the division funneled cases to this specialist, thereby concentrating our collective experience into this surgeon, who then became the champion for cutting-edge technology and advanced endovascular techniques. Every complex EVAR was performed with the referring surgeon and the dedicated specialist surgeon as cosurgeons. This strategy of concentrating experience to support the initial development of expertise led to a rapid accumulation of case volume along with the skill set, which was then shared with the rest of the group (Figure 1).
An exponential increase in case volume of type A aortic dissections* has allowed our open arch experience to grow and mature. Expertise in arch reconstruction involves multiple skill sets obtained through repetition. These cases may not be part of a typical cardiac surgery training experience and therefore are often beyond the scope of most cardiac surgeons’ expertise. The Society of Thoracic Surgeons reported that only 20% of centers perform more than five type A repairs annually.4 Better outcomes associated with high-volume centers have been demonstrated in TEVAR, with 40 or more cases per year resulting in superior patient outcomes.5 By comparison, we perform approximately 80 type A repairs per year, and our graduates finish their training with 25 cases. Refinement of technical skill as well as improved knowledge of multiple perfusion models and a dissection-specific critical care protocol resulted in improved patient outcomes. Developing expertise in treating patients with type A aortic dissection has expanded our willingness to offer open repair to more patients with challenging anatomy and/or a high-risk comorbidity profile. Cases that were once sent away to specialized centers are now referred to our center for repair.
Dedicated Training
The dedicated specialist surgeon then spent 3 months of sabbatical at another high-volume center to further refine technical skills and the workflow of complex endovascular aortic procedures. This translated to an immediate improvement in technical efficiency and operating room workflow during complex EVAR, as evidenced by the increased number of target vessels, while decreasing total fluoroscopy time, and contrast used (Figure 2).
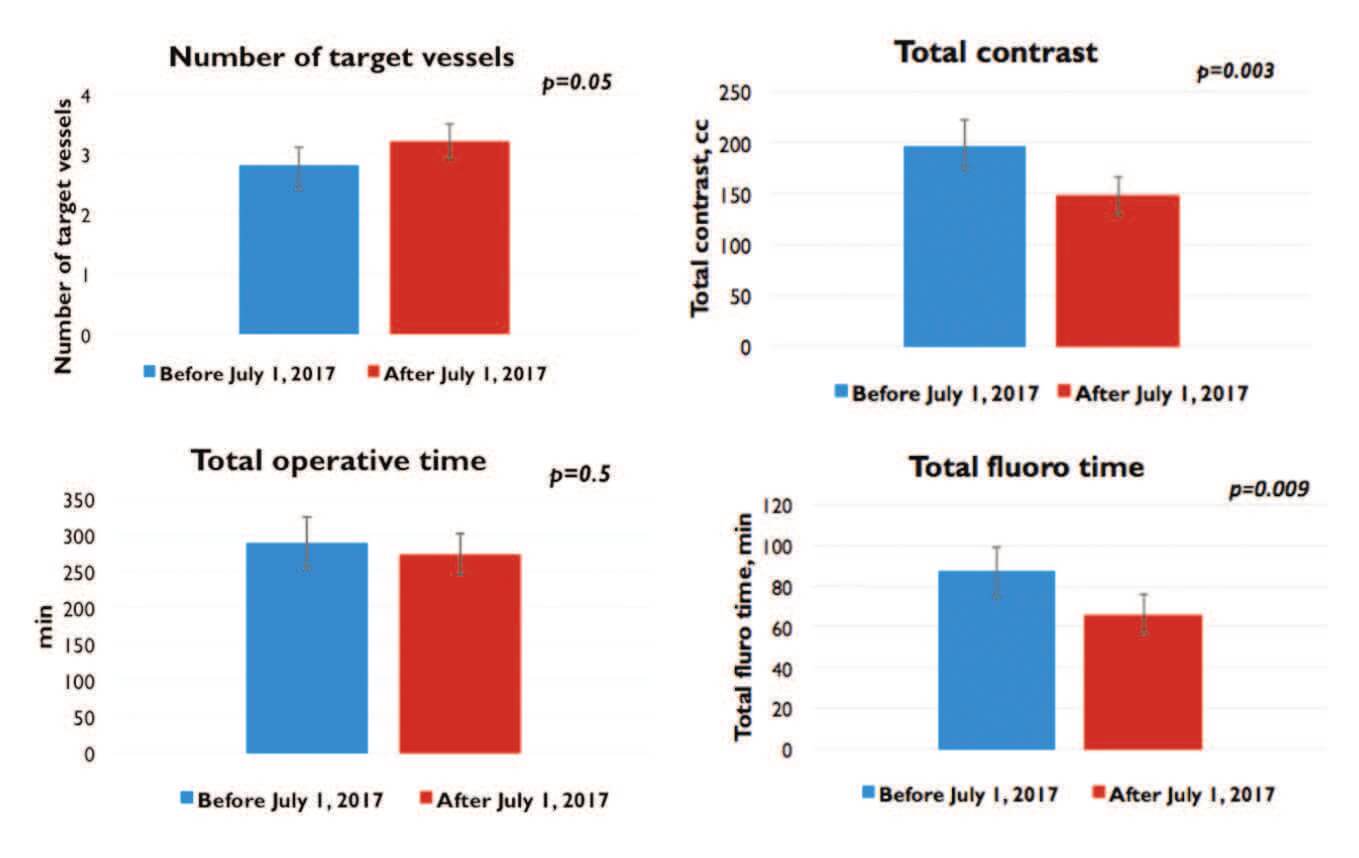
Figure 2. Impact of dedicated additional training in complex EVAR. We were able to increase the number of target vessels during complex EVAR, while reducing the amount of contrast and the fluoroscopy time.
*Cook Zenith Dissection System is not indicated for use in type A dissections.
2. DEDICATED AORTIC HOTLINE AND RAPID TRANSPORT SYSTEM
We aimed to develop a system that could overcome the delay caused by the multitude of logistical steps involved in a typical transfer process of aortic dissection patients. A rapid transport system dedicated to aortic emergencies is our solution to this issue. The transport team consists of an aortic hotline operator, nurse practitioner, administrative assistants, and on-call vascular and cardiac surgeons. A call schedule specific to aortic emergencies is shared among vascular and cardiac surgeons. All calls received by the aortic center hotline are immediately evaluated by the on-call cardiac or vascular surgeon. Following the surgeon’s acceptance for transfer, the administrative assistant arranges land or air transport. Mode of transport is primarily determined on the basis of the distance from the referring center to ours and also by acuity. While the patient is en route, the accepting surgeon and administrative assistant activate the intensive care unit team as well as the operating room team, which includes the on-call cardiac anesthesiologist and, depending on the incoming emergency, on-call perfusionist or radiology technologists. On arrival, all patients are directly admitted to the intensive care unit, where the patient is assessed and the need for operation is rapidly determined. This system is designed with the goal of transferring any patient with an acute aortic emergency from a sending facility to the Keck Hospital intensive care unit within a 2-hour time frame (Figure 3).
Figure 3. Workflow of our aortic hotline and rapid transport system.
This approach differs from a typical transfer process in three ways. First, the call bypasses the on-call house officer, who may be busy with inpatient issues or may be operating when these aortic emergency transfer requests are received. Having direct access to the on-call attending who can make immediate decisions facilitates expeditious treatment of these patients. Second, a dedicated aortic call schedule for the attending surgeons that is entirely separate from the general call schedule improves the attending response time by reducing the chance of the on-call attending being inundated with other emergencies. Third, we have contracted with ambulance and helicopter services, which enables immediate arrangement of transportation. The onus of arranging for transportation is lifted from the referring hospitals. Implementation of this system combined with outreach efforts, as outlined in the following section, have resulted in significant growth in the number of aortic emergency cases we have received (Figure 4).
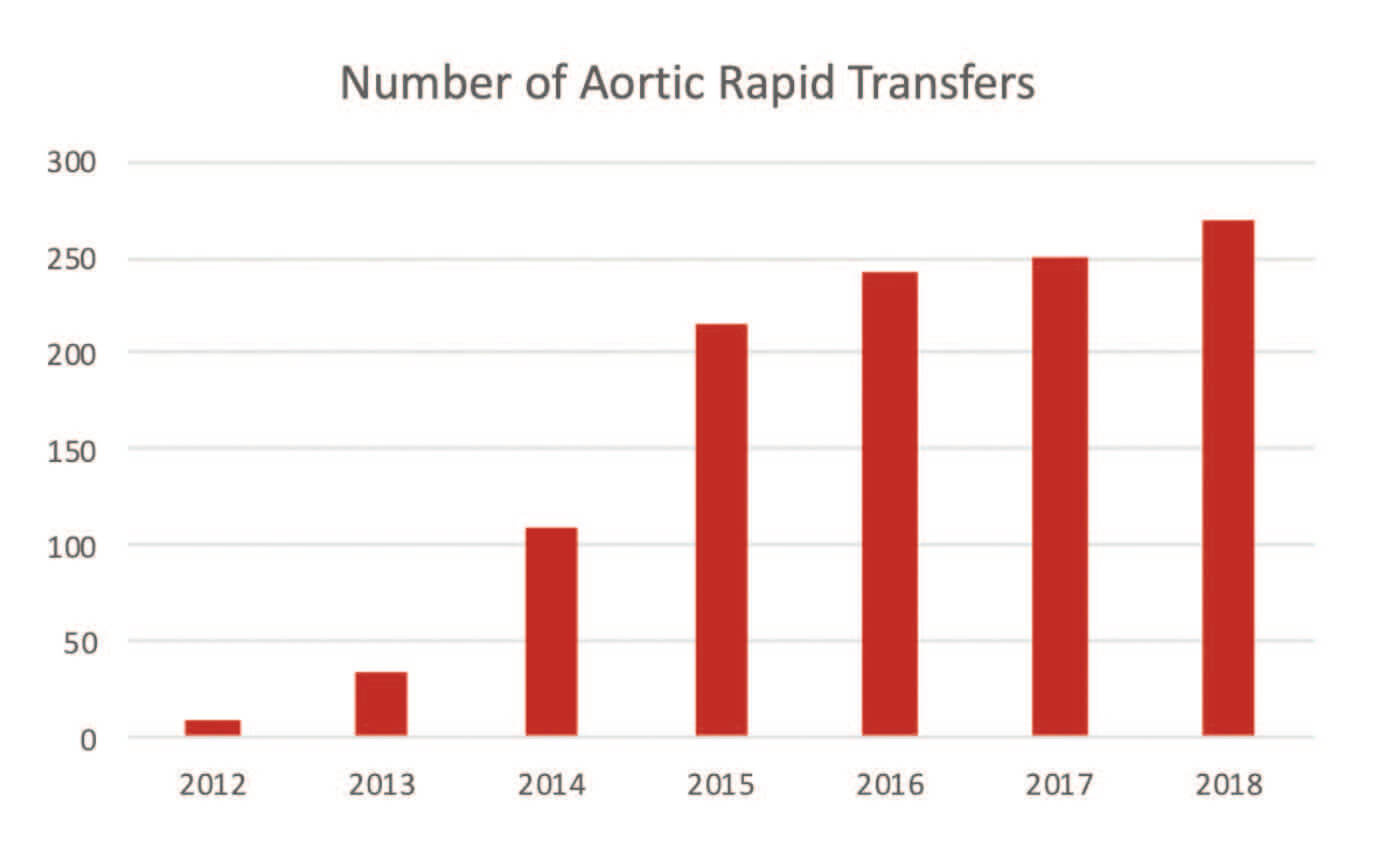
Figure 4. Growth of our aortic emergency case volume by year.
3. RAISING REGIONAL AWARENESS THROUGH OUTREACH
The goal of our outreach was improving awareness of the importance of rapid and accurate diagnosis of aortic dissections in the emergency department setting, as well as the availability of the previously mentioned aortic hotline and rapid transport system. As part of our outreach, we focused on small- to medium-size emergency departments, as we thought these centers were most in need. These centers often do not have readily available access to cardiac or vascular surgeons who routinely handle aortic emergencies. We also found that more centers had vascular on-call services but lacked cardiac on-call services.
Differentiating between ascending, arch, or descending aortic pathologies was often difficult, resulting in misdiagnosis and mistreatment. Therefore, we found that emergency department physicians were very eager to incorporate our services into their algorithm. In our experience, center or regional politics seldom prevented engagement.
4. DEVELOPMENT OF MULTIDISCIPLINARY AORTIC CENTER CONFERENCES
Members of aortic center conferences include vascular surgeons, cardiac surgeons, cardiovascular radiologists, dedicated nurse practitioners, and aortic research fellows. The conferences are centered around case discussions, where management options and surgical plans are formulated. This conference has also been a useful venue for discussing new technology and reviewing the latest literature affecting the treatment algorithm of aortic pathologies.
5. DEVELOPMENT OF A MULTIDISCIPLINARY FOLLOW-UP CLINIC AND SURVEILLANCE PROGRAM
Beyond the acute phase of aortic dissections, patients should be followed over their lifetime with serial surveillance imaging. Regardless of the treatment they underwent during the acute phase (medical, open surgical, or endovascular repair), a systematic surveillance program serves as an integral part of an aortic center to optimize the long-term outcomes. Growing evidence suggests that a significant portion of patients develop abdominal aneurysmal degeneration in the long term after TEVAR for aortic dissections.6 Detection of early signs of failure or negative remodeling should trigger an individualized treatment plan for each patient to prevent catastrophic aortic events. A multidisciplinary follow-up clinic where patients can be seen by vascular and cardiac surgeons, as well as antihypertension specialists, offers convenient, comprehensive care. In our experience, this patient-centered arrangement also improves patient satisfaction and compliance with the surveillance program.
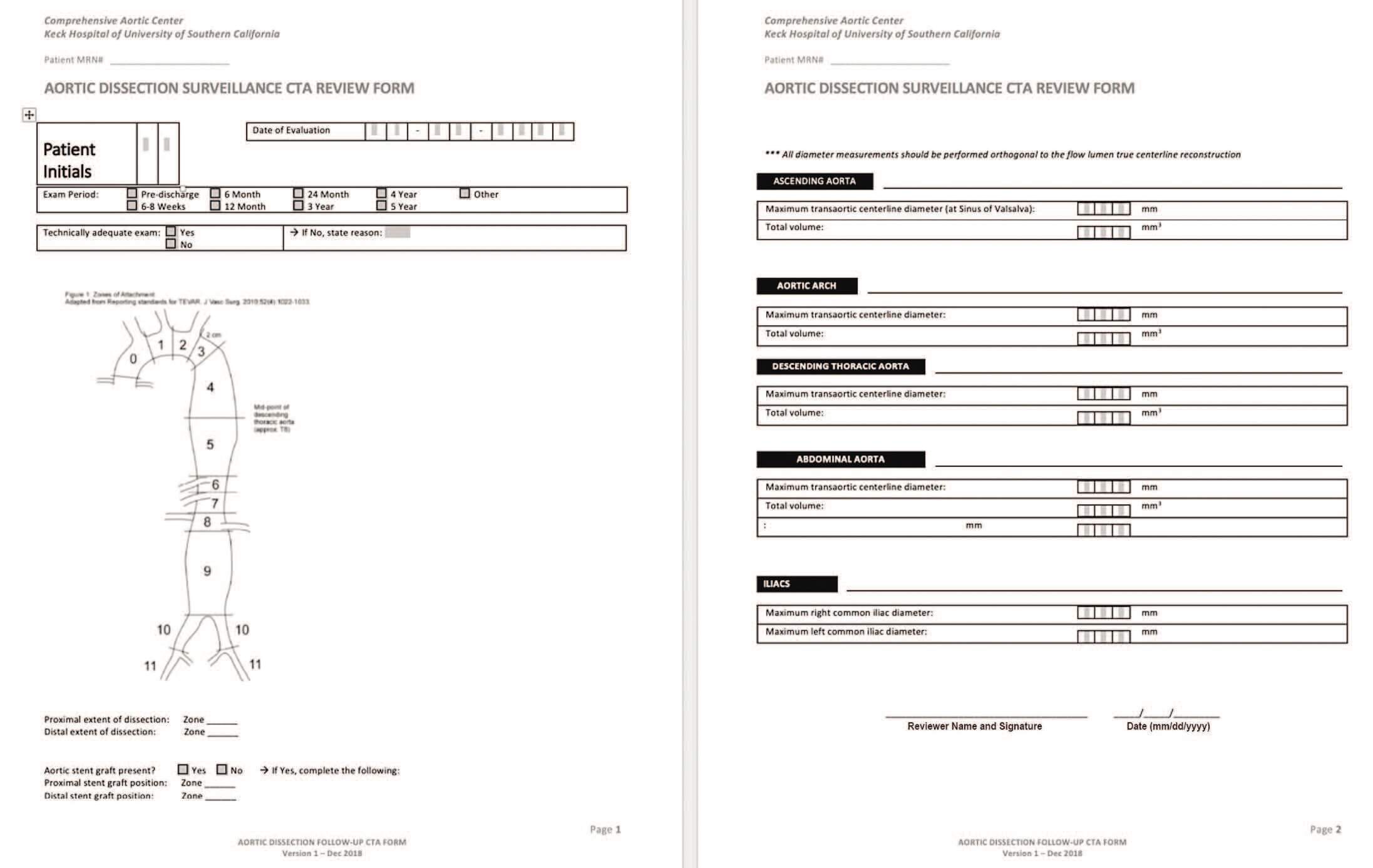
Figure 5. Standardized form for our aortic dissection imaging surveillance program.
Additionally, we have implemented a standardized aortic image surveillance program whereby the dedicated cardiovascular radiologists perform centerline and volume measurements in different aortic segments (Figure 5). These measurements provide a consistent tool to detect aortic dilatation.
COMMON ROADBLOCKS
Challenges to forming a truly collaborative partnership lie more often in the physicians rather than the patients. Concern for not receiving due credit (financial or otherwise) during a joint case, disagreement regarding treatment plan, as well as the desire to keep the skill set siloed are some of the common roadblocks and are rarely in the patients’ interests. Sentiments such as, “This is my patient,” “I should get the credit,” “They don’t have the skill set,” “I am the real surgeon,” and “Why should I teach them?” are counterproductive to the optimal care of patients with aortic dissections.
Overcoming these roadblocks requires recognition of overlapping pathologies that can be treated using different approaches, the value of nonoverlapping skill sets offered by different disciplines, and finally the willingness to share and learn from each other with the common goal of achieving the best possible patient outcome. At the outset of our aortic center, we formed an agreement that every TEVAR will be performed with both cardiac and vascular surgeons scrubbed. The primary attending in charge of the patient undergoing TEVAR is the primary surgeon billing for the case, while the counterpart bills for the adjunctive procedures such as branch stenting, and as an assistant for the index TEVAR. With this agreement and the robust growth of our total volume, financial concerns regarding these cases disappeared. Additionally, this approach more than doubled the TEVAR experience for our trainees in cardiac and vascular programs. Going through challenging cases and managing complications together, we saw mutual respect and a collaborative spirit grow and solidify.
CONCLUSION
Aortic dissections can be challenging to manage because of the complex pathology that patients can present, as well as the wide array of treatment options. Management of aortic dissections continues to evolve with rapid technical and technological refinement. As such, optimal care of aortic dissection patients involves a multidisciplinary approach with expertise in medical, open surgical, and endovascular treatments. A successful aortic center begins with a synergistic partnership between multidisciplinary specialists dedicated to aortic care, with vascular and cardiac surgeons as “co-captains” of the team. With this foundation, the five components discussed in this article to ensure the success of an aortic center can be implemented to deliver optimal care to aortic dissection patients. With growth of the aortic center and collective experience, mutual respect will solidify and help create a truly collaborative partnership.
Sukgu Han, MD, MS
Co-director to the Comprehensive Aortic Center
Keck Medical Center
University of Southern California
Division of Vascular Surgery and Endovascular Therapy
University of Southern California
Los Angeles, California
sukgu.han@med.usc.edu
Disclosures: Proctor, speaker, and consultant for Cook Medical; consultant for WL Gore and Associates.
Fernando Fleischman, MD
Co-director to the Comprehensive Aortic Center
Keck Medical Center
University of Southern California
Division of Cardiothoracic Surgery
University of Southern California
fernando.fleischman@med.usc.edu
Disclosures: Proctor, speaker, and consultant for Cook Medical; consultant and principal investigator for WL Gore and Associates; consultant and principal investigator for Terumo/Bolton.
- Vilacosta I, San Román JA. Acute aortic syndrome. Heart. 2001;85:365-368.
- Tsai TT, Nienaber CA, Eagle KA. Acute aortic syndromes. Circulation. 2005;112:3802-3813.
- Manzur M, Han SM, Dunn J, et al. Management of patients with acute aortic syndrome through a regional rapid transport system. J Vasc Surg. 2017;65:21-29.
- D’Agostino RS, Jacobs JP, Badhwar V, et al. The Society of Thoracic Surgeons Adult Cardiac Surgery Database: 2018 update on outcomes and quality. Annals Thorac Surg. 2018;105:15-23.
- Gazoni LM, Speir AM, Kron IL, et al. Elective thoracic aortic aneurysm surgery: better outcomes from high-volume centers. J Am Coll Surg. 2010;210:855-859.
- Famularo M, Meyermann K, Lombardi JV. Aneurysmal degeneration of type B aortic dissections after thoracic endovascular aortic repair: a systematic review. J Vasc Surg. 2017;66:924-930.