Benefits of Zilver Vena
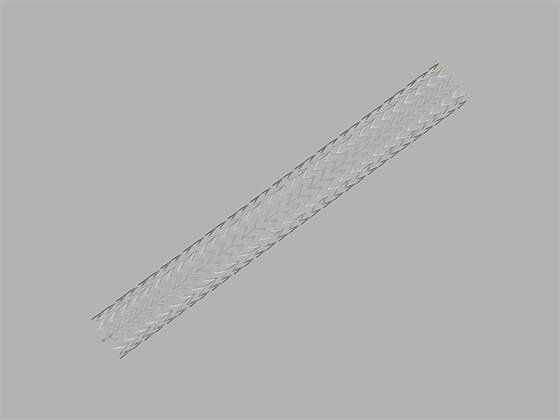
Zilver Vena holds open the iliac and femoral veins, which helps blood flow normally back to the heart. This may help reduce symptoms such as leg pain and swelling.
Zilver Vena was evaluated in the VIVO Clinical Study which included 243 patients. Overall, patients had good outcomes. The results of the study showed that patients who received a Zilver Vena stent reported having fewer symptoms of iliofemoral venous outflow obstruction. The study also showed that the stent helped to maintain blood flow back to the heart.1
Who should not receive a Zilver Vena Venous Self-Expanding Stent?
Before a stent placement, your doctor will determine if you are a candidate for the Zilver Vena Venous Self-Expanding Stent. The Zilver Vena Venous Self-Expanding Stent should not be used in patients who:
- have a lesion that prevents crossing or complete inflation of a venoplasty balloon or proper placement of the stent or stent delivery system
- cannot receive specific blood-thinning medications, such as aspirin or Coumadin, among others
Risks
Placement of a Zilver Vena stent has some risks*, including, but not limited to:
- Abdominal or back pain
- Abrupt stent closure
- Allergic reaction to anticoagulant and/or antithrombotic therapy or contrast medium
- Allergic reaction to nitinol (nickel-titanium)
- Amputation
- Aneurysm
- Arrhythmia (abnormal heartbeat)
- Arteriovenous fistula (AVF; an abnormal connection between a vein and artery)
- Bleeding associated with anticoagulation
- Death
- Embolism (a clot that has migrated and blocks blood flow in a vessel)
- Fever
- Hematoma (a collection of blood trapped in a tissue layer) and/or hemorrhage (excessive loss of blood) at access site
- Hypersensitivity reactions
- Hypertension (a blood pressure that is higher than normal)
- Hypotension (a blood pressure that is lower than normal), nausea, or symptoms of a vasovagal response (a nervous system reaction causing slow heartbeat, low blood pressure, and potentially fainting)
- Infection and/or abscess (a collection of pus in a tissue) formation at the access site
- Intimal (inner lining of a vessel) injury and/or dissection (a separation of vessel layers)
- Myocardial infarction (MI) (heart attack)
- Pseudoaneurysm (large opening or dilation of an artery, giving the appearance of a rupture) formation
- Pulmonary embolism (a clot that has migrated and blocks blood flow in an artery of the lung)
- Renal (kidney) failure
- Restenosis (recurrence of a narrowed vessel or stent), occlusion (blockage), or thrombosis (blood clotting) of the stented vein
- Septicemia (a blood infection) and/or bacteremia (bacteria in the blood)
- Stent malapposition (separation of a stent from the inner lining of the vessel wall)
- Stent migration or embolization
- Stent strut fracture
- Stroke (damage to brain tissue from limited blood flow to the brain or bleeding in the brain)
- Tissue necrosis (tissue death)
- Vasospasm (sudden contraction of the muscular walls of an artery)
- Vessel perforation and/or rupture (the bursting of a blood vessel)
- Worsened pain
*Talk to your doctor if you have concerns or questions.
Before and after your Zilver Vena placement
What to expect before your procedure:
Your doctor will tell you how to prepare for your stent placement.
What to expect after your procedure:
When your procedure is finished, you will go to a recovery area. You may feel some pain and may be given pain-relief drugs. Nurses will closely monitor your blood pressure and heart rate. Your doctor will decide when you can go home and when it is okay for you to resume normal activity.
Your doctor may prescribe blood thinners after you receive your stent. These drugs help prevent blood clots from forming.
Patients in the Zilver Vena VIVO Clinical Study1 were prescribed an anticoagulant (blood thinner) for at least six months in addition to an aspirin (antiplatelet) for the duration of the study.1 Ask your doctor what drugs are being prescribed, and don’t stop taking these drugs without your doctor’s approval. Please remember, as with any surgery or medical procedure, the best source of information and advice is your doctor. It is important to follow your doctor’s instructions and to come back to be evaluated by your doctor.
- Summary of safety and effectiveness data (SSED): Zilver Vena Venous Self-Expanding Stent. Food and Drug Administration Web site. http://www.accessdata.fda.gov/cdrh_docs/pdf20/P200023B.pdf Accessed September 8, 2021.